What are sleep disorders?
Sleep disorders are health conditions that affect the quality, amount, and timing of sleep that a person gets. Sleep disorders often lead to sleep deficiency and are common among adults.
Click the dropdowns below to read more about common sleep disorders. To learn more about sleep disorders, you can visit the CDC’s website1. If you feel that your sleep is inadequate, please talk to your health care provider.
Chronic insomnia occurs when a person has difficulty initiating sleep or waking too early in the morning for 3 or more times a week for 3 months or more and is not explained by another health problem. Around 30% of the adult population are affected by chronic insomnia and 10% have insomnia that affects daytime function.
Treatments for Insomnia
Cognitive Behavioral Therapy for Insomnia (CBTI)
- CBTI addresses behaviors, cognitions, and perceptions (perpetuating factors) that lead to problems with falling asleep, staying asleep, or awakening too early in the morning.
- CBTI can have equal or better effects than drugs and can have longer-lasting effects.
- There are minimal side effects to CBTI compared to using drugs.
CBTI can be conducted in individual or group sessions, via face-to-face, telehealth, or online formats, including “apps”). Some people may benefit from brief (2 sessions) or longer sessions (up to 8 weeks). It is led by trained therapists (psychologists, physicians, or nurses). It has best effects when participants learn and practice the methods provided in these sessions.
Medications
Prescription Medications
There are several groups of medications that may be prescribed for insomnia including:
- Hypnotic medications
- Psycho-active medications with sleepiness as a side-effect
- E.g. Trazadone, amitriptyline, doxepin, trimipramine, mirtazapine, olanzapine, quetiapine
- Anticonvulsant medications
- E.g. Gabapentin, pregabalin
- Melatonin receptor agonists
- E.g. Ramelteon
- Other
- E.g. Chloral hydrate, Sodium oxybate
Side effects of prescription medications might include lightheadedness, headache, diarrhea, upset stomach, daytime sleepiness, memory issues, and thoughts about self-harm. Talk to your health care provider if you have questions about prescription sleeping medications.
Over-the-Counter Medications
There are over-the-counter medications that can also help with sleep:
- Melatonin
- Antihistamines (see examples below)
- Diphenhydramine (Benadryl) –
- Herbal remedies
- E.g. Valerian
Side effects might include headache, upset stomach, weakness, daytime sleepiness, dry mouth, constipation, and trouble emptying bladder. Talk to your health care provider if you have questions about over-the-counter medications.
Store brands of medications containing the same active ingredients as brand names have the same risks and benefits and are often less expensive than the brand name version.
Precautions
- Start with your health care provider. Ask your health care provider if the sleep aid might interact with other medications or underlying conditions. Also ask what dosage to take.
- Keep precautions in mind. Diphenhydramine and doxylamine aren’t recommended for people who have certain health problems, including closed-angle glaucoma, peptic ulcer and urinary retention. In addition, sleep aids pose risks for women who are pregnant or breastfeeding, and might pose risks for people over age 65, including an increased risk of dementia.
- Take it one day at a time. Nonprescription sleep aids might be a temporary solution for sleep problems. However, they’re not intended for long-term use.
- Avoid alcohol. Never mix alcohol and sleep aids. Alcohol can increase the sedative effects of the medication.
- Beware of side effects. Don’t drive or attempt other activities that require alertness while taking sleep aids.
- Many over-the-counter medications contain antihistamines. The longer you take them, the less likely they are to make you sleepy.
Visit MayoClinic.org Sleep Aids Information to learn more about other ways to treat insomnia.
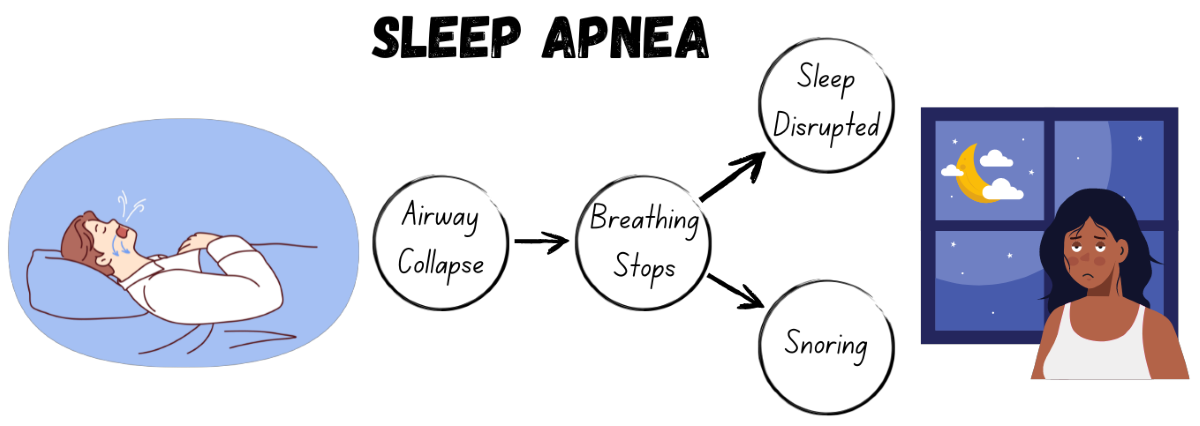
Obstructive sleep apnea (OSA) occurs when the airway is repeatedly blocked at night. Some symptoms of OSA include snoring, choking or gasping during sleep, and fatigue or daytime sleepiness. Over 20% of adults suffer from it. OSA affects 15-30% of men and 10-15% of women. Men are more likely to have OSA than women until women reach menopause, after which both genders have equal rates. Individuals who have OSA have a higher risk of OSA. OSA contributes to significant health issues, such as diabetes, heart disease, and stroke. Many people have OSA and don’t know it. Let your health care provider know if you have loud snoring, frequent awakenings, stop breathing, or gasping during your sleep.
Treatments for Obstructive Sleep Apnea
- Continuous Positive Airway Pressure (CPAP)
- A CPAP machine can reduce apneas and hypopneas and improve sleepiness, however, adherence to using the machine regularly can be difficult.
- Weight loss
- Oral appliance
- Surgery on upper airway
- Hypoglossal nerve stimulation
Restless leg syndrome (RLS) is a neurological disorder triggered by rest and is characterized by uncomfortable sensations in the legs, resulting in an irresistible urge to move them. Symptoms are more prevalent in the late afternoon or evening and peak at night. Experts estimate that 7-10% of the U.S. population may have RLS.
Treatments for RLS
While there is no cure for RLS, medications and lifestyle changes can help alleviate symptoms.
Prescription Medications
There are several groups of medications that may be prescribed for RLS including, but not limited to
- Iron supplements
- Anti-seizure medications
- Dopaminergic agents
Lifestyle Changes
There are several lifestyle changes that may be recommended for RLS including, but not limited to
- Avoid or decrease the use of alcohol, nicotine, and caffeine
- Change or maintain a regular sleep pattern
- Try moderate, regular exercise
- Massage the legs or take a warm bath
- Apply a heating pad or ice pack
- Use foot wraps specially designed for people with RLS, or vibration pads to the back of the legs
- Do aerobic and leg-stretching exercises of moderate intensity
1Reference to specific commercial products, manufacturers, companies, or trademarks does not constitute its endorsement or recommendation by the U.S. Government, Department of Health and Human Services, or Centers for Disease Control and Prevention. This material is otherwise available on the agency website for no charge.